
Madi Garst (left) with Bridges Health, and Tanecia Davis, CPO's Director of Workforce Development, share a table at the recent Employers in Action Day at the State Capitol.
Employers in Action Day focuses on need to balance economic growth with sustainable environment
Talent Acquisition Specialist at Bridges Health
On Wednesday, March 26, I had the honor of attending Employers in Action Day at the Oklahoma State Capitol. Organized by the State Chamber, Employers in Action is a coalition of employment professionals and business leaders who are committed to keeping the HR community informed and engaged in the legislative process. At this event, employers from across the state heard legislators emphasize the need to balance economic growth with a sustainable environment for Oklahoma businesses.
Representative Mark Tedford began the day. He spoke with us about House Bill 1161, warning that healthcare mandates can unintentionally function as taxes on small businesses. While the bill only has general support in the House, it's important for our long-term care industry to be aware of legislation that could add costs to our already strained budgets. Representative Brian Hill, Chair of the new Economic Development Committee, was excited to speak to us about Oklahoma’s economic potential, proudly saying, "I believe Oklahoma is at its greatest moment." Hill discussed workforce development in the “Big Tech” industry and his commitment to keeping the next generation of the working class in Oklahoma rather than losing them to our Texas neighbors. Senator Julie Daniels is also focused on pro-business legislation, particularly in regards to workers' compensation. Her goal is to fine-tune legislation to rehabilitate injured employees and return them to work as efficiently and timely as possible, while protecting business owners from unnecessary fees.
State Question 832: The $15 Minimum Wage Initiative
Next up for discussion was State Question 832. The “$15 Minimum Wage Initiative” plans to gradually raise the minimum wage in Oklahoma from the current $7.25 per hour to $15 per hour by 2029. Adam Maxey, VP of Government Affairs, noted that although only 2% of Oklahoma’s workforce currently earns $7.25 per hour, the larger concern lies in the domino effect this would have on businesses and the price of goods. For long-term care facilities and providers, this initiative could dramatically impact overall cost of care.
Maxey noted that minimum wage increases in California led to widespread layoffs. For long-term care providers (who are already fighting for adequate state funding), this mandate could result in staff layoffs or even closures if additional funding isn’t found elsewhere. While the economic impact data is still coming in, long-term care providers should prepare for the potential cascading effects this initiative would cause after the June 2026 voting occurs.
● Competency-Based Post-Secondary Programs would allow students to graduate by demonstrating a “mastery” of their skills/degree, rather than simply completing the traditional required courses.
Additionally, legislators are working on lowering ambulance service costs, which I see as an indirect (but helpful) benefit for long-term care residents who sometimes require emergency transportation.

Justin McGrew introduces Sen. Brenda Stanley from Midwest City to ICF Day at the Capitol participants
We brought 150 clients and staff to OKC to make impactful statement on the benefits of ICF/IID facilities
Editor's note: Justin McGrew, chairman of CPO's Board of Directors, operates a mix of ICF and nursing facilities across Oklahoma through Sallisaw-based ONHL Health Services. Justin wrote this blog to share his perspective on the recently completed ICF/IID Day at the Capitol, and its importance to ICF communities and their clients across the state.
By Justin McGrew
CPO Chairman of the Board
CPO's 3rd annual ICF/IID Day at the Capitol brought a buzz of excitement to the second floor Rotunda on March 11th. It was a feel-good event with the purpose of showcasing to state legislators our client communities and the vocational skills they have learned.
Tables were set up throughout the Rotunda, highlighting ICF facilities from across the state, with posters decorated with pictures and drawings, telling the stories of each community. The Clients, most of whom traveled long distances to participate in ICF Day at the Capitol, enthusiastically greeted visitors who wanted to know more throughout the day.
If you aren't familiar with ICF/IID -- Intermediate Care Facilities for Individuals with Intellectual Disabilities -- they are communities of anywhere from 16 to 150 clients, and they provide far more than just food, shelter and medical care to some of the state's most vulnerable citizens.
Beyond the care component, we are dedicated to helping our clients become as successful and independent in life as possible, whether that is simply navigating the activities of daily living or as complex as working in an off-campus job in town. In fact, many of our clients receive advanced levels of 'pre-vocational’ skills training that allow them to interview and gain employment in their local community.
 We have a lot of clients that work in the food industry, deliver newspapers, stock shelves, work in retail shops, perform maintenance, laundry, lawncare and housekeeping services. We even have communities that shuttle clients on a 15-mile one way commute each day to farm in a large vegetable gardening center. Another great example was on full display at our Capitol Day, as one of our client communities designed and produced beautiful and colorful T-shirts that were worn by all the attendees. These are just a few examples of the workforce impacts our clients have in their respective communities.
We have a lot of clients that work in the food industry, deliver newspapers, stock shelves, work in retail shops, perform maintenance, laundry, lawncare and housekeeping services. We even have communities that shuttle clients on a 15-mile one way commute each day to farm in a large vegetable gardening center. Another great example was on full display at our Capitol Day, as one of our client communities designed and produced beautiful and colorful T-shirts that were worn by all the attendees. These are just a few examples of the workforce impacts our clients have in their respective communities.
After the Rotunda showcase on ICF Day at the Capitol, the entire party of approximately 150 people moved to lunch on the Capitol's first floor where they had the opportunity to hear from five state legislators and a representative of the Oklahoma Health Care Authority. Thank you to Senators Kelly Hines, OKC; and Brenda Stanley, Midwest City; as well as Representatives Josh Cantrell, Kingston; Ryan Eaves; Atoka; and Forrest Bennett, Oklahoma City; for taking time out of their busy day to share their thoughts with our ICF members.
ICF Day at the Capitol certainly didn't end with lunch. After a great meal and inspiring words from our legislative visitors, many participants and facility staff members went upstairs to visit individual legislators and sit in the gallery to watch some floor debates.
It was a long and fast paced day, but as our ICF clients left the Capitol to board buses for their trips back home, I knew it was successful and a worthwhile event by the smiles on their faces. Thank you all for participating.
With respect to our mission, we can't always assume that our local legislators understand what we do on a daily basis, as they are extremely busy and often unfairly expected to know everything about every type of business in their respective district. Our ICF Day at the Capitol, along with ongoing visits from other Long Term Care facilities across the state, are designed to educate and reiterate what we do in our communities and make the case for adequate funding to sustain our operations.
Our ICF communities are specifically urging legislators to fund ICF/IID facilities at 112% of cost. That level of funding will enable us to invest in equipment and programs used to provide new skills and employment to our Clients, as well as a continued investment into our staff members and our buildings.
My message to all Oklahoma Long Term Care operators is this: the most important thing we can do right now is to get out of our communities and go visit with our legislators in their offices, telling our stories and advocating for adequate funding.
Remember, there are no wasted days at the Capitol!

A view of the Rotunda with displays showcasing ICF Facilities

Participants in recent workforce roundtable at SideXSide OKC listen as a speaker shares info on helping job seekers overcome employment obstacles
Workforce professionals, supporting organizations gather at SideXSide OKC
By Tanecia Davis
Workforce Development Director
Earlier this week, I had the opportunity to attend a workforce roundtable hosted by SideXSide OKC and the Greater OKC Chamber. This first of many quarterly meetings to bring together workforce professionals, organizations, and employers to discuss ways to better support Oklahomans facing employment barriers.
🔹 The benefits of SideXSide participants and job fairs in bridging the employment gap
🔹 Addressing background check challenges and the need for employer flexibility.
🔹 How organizations embedding essential skills into their programs see higher success rates.
🔹 A map of nonprofits to help direct job seekers to the right resources.
🔹 Employers improving turnover rates by adjusting hiring and retention processes.
🔹 SideXSide’s 87% retention rate — a testament to the power of holistic workforce development!
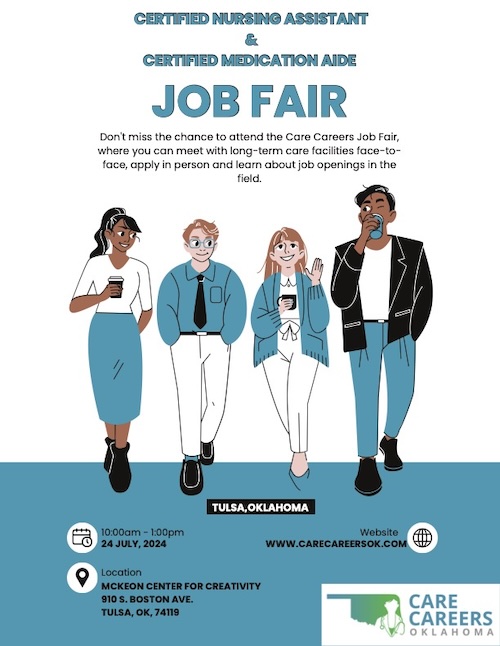
Don't miss this opportunity to connect with potential new Long Term Care workers

We're expanding Care Careers workforce development program to include Developmentally Disabled Care Aides

Tanecia Davis, CPO's Director of Workforce Development
I've got some exciting updates to share about our Care Careers Oklahoma workforce development program.
Elevate program designed to prepare next generation of leaders in Long Term Care
FOR IMMEDIATE RELEASE
 Jan. 7, 2025
Jan. 7, 2025
MEDIA CONTACT:
Alex Weintz, aweintz@amberintegrated.com
OKLAHOMA CITY — Care Providers Oklahoma is proud to announce the launch of its innovative training program, "Elevate: Excellence in Nursing Home & Long-Term Care Administration," designed to prepare the next generation of leaders in long-term care.
The Elevate program combines comprehensive classroom instruction with practical, hands-on experience to equip participants with the skills and knowledge necessary to succeed as long-term care administrators. Spanning seven classroom sessions over 19 weeks, the program covers critical areas such as regulatory compliance, leadership strategies, budgeting, staff management, and communication skills.
“This program represents a significant step forward in ensuring that Oklahoma’s nursing homes and long-term care facilities are led by knowledgeable and compassionate administrators,” said Natashia Mason, Director of Strategic Initiatives for Care Providers Oklahoma. “Elevate is designed to provide both the theoretical knowledge and practical tools necessary to excel in this vital field.”
Graduates will be fully prepared to meet state licensing requirements and confidently pursue careers as Tier 1 Long-Term Care Administrators. The program also includes an optional National Association of Long-Term Care Administrator Boards (NAB) review to help participants prepare for certification exams.
The first cohort begins on January 27, 2025, with a second cohort launching in June. Enrollment for the January cohort closes on January 23, 2025.
For more information or to enroll, visit www.careoklahoma.com and navigate to the Education section or contact Natashia Mason at the information below.
Contact:
Natashia Mason
Care Providers Oklahoma
Email: Natashia@careoklahoma.com
Phone: (405) 524-8338 x 101
OIG Releases Nursing Facility Compliance Program Guidance
When not performed accurately, Medication Reconciliation can lead to medication errors

Angie Hamer
By Angie Hamer, RN, RAC-CT
Senior Consultant, Proactive LTC Consulting
Medication Reconciliation, when not performed accurately, can lead to medication errors. These errors often occur during a resident’s transition or transfer to another level of care, admission to the facility, or at the time of discharge.
Common causes include:
- Performance deficits
- Inaccurate or omitted transcription
- Poor Documentation
- Ineffective Communication
- Workflow disruptions
- Examples of Medication Errors Include:
- Incorrect dose or quantity
- Omission errors
- Prescribing errors
- Wrong drug
- Wrong time
- Extra dose
- Wrong patient
- Mislabeling
- Incorrect administration technique
- Wrong dosage form
Let’s consider the “who, what, when, why, and how” of medication reconciliation.
- Medication reconciliation is a systematic review of a resident’s complete medication regimen, including:
- Prescribed and over-the-counter (OTC) drugs.
- Nutritional supplements, vitamins, herbal, and homeopathic products.
- Specialized treatments such as total parenteral nutrition (TPN) and oxygen therapy.
- This process aims to identify and resolve clinically significant issues like duplicate therapies, adverse drug interactions, improper dosages, or medications without a clear indication for use.
- Health-Related Quality of Life
- Medication-related errors are common, particularly during transitions of care, and can lead to serious harm, emergency visits, rehospitalizations, or even death.
- Adverse outcomes not only threaten physical health but also compromise the overall quality of life.
- Safety and Continuity of Care
- By identifying and addressing medication errors at admission, during a resident’s stay, and upon discharge, medication reconciliation mitigates risks.
- Providing a reconciled medication list during transitions improves care coordination and enhances resident safety.
- At Admission: Conducted as close to the time of admission as possible to identify potential issues.
- Throughout the Stay: Ongoing monitoring ensures medication regimen remain safe and effective.
- At Discharge: A reconciled medication list is provided to subsequent care providers to facilitate a smooth transition and avoid errors.
- A collaborative team effort is essential:
- Healthcare Providers and Pharmacists: Conduct comprehensive reviews and resolve issues.
- Nursing Staff: Administer medications and monitor for adverse effects.
- Residents and Families: Provide critical information about medication histories and adherence.
- Steps for Effective Medication Reconciliation
- Conduct a Comprehensive Drug Regimen Review
- Review medical records, transfer documents, and discharge summaries.
- Discuss medication details with healthcare professionals, residents, and family members.
- Identify Clinically Significant Issues
- Allergies or adverse reactions.
- Incorrect dosages or frequencies.
- Serious drug interactions (drug-drug, drug-food, or drug-disease).
- Omission of necessary medications or inclusion of unnecessary ones.
- Include active, held, and discontinued medications with detailed information (e.g., dosage, timing, and special instructions).
- Ensure the list is customized to the resident’s specific needs and subsequent care requirements.
- Educate and Train Staff
- Train staff on proper medication administration and monitoring for adverse effects.
- Develop systems to promptly evaluate and address medication issues.
- Medication reconciliation is essential for reducing medication errors, improving safety, and enhancing the quality of care.
- A proactive, team-based approach ensures potential issues are addressed promptly, minimizing resident risk.
- Clear communication during transitions of care, including providing a reconciled medication list, plays a critical role in sustaining effective treatment and continuity.
- By focusing on the “who, what, when, why, and how,” healthcare facilities can integrate medication reconciliation into routine care, ensuring that every resident receives the safest and most effective treatment possible.
- Access on-demand training on assessing risk and implementing safeguards to prevent medication errors

McMahon Tomlinson Nursing & Rehab staff proudly show off their 2024 AHCA/NCAL Bronze Quality award.
'Winning the Bronze Award inspired us to strive for even higher standards'
Editor's Note: McMahon Tomlinson Nursing & Rehab in Lawton was one of 13 Oklahoma AHCA/NCAL Bronze Quality Award winners for 2024. We asked Administrator and Oklahoma Leadership Academy alum Stacy Forrest to write the following post about the experience of submitting the application and how it impacted the McMahon Tomlinson residents, its team and the care they provide at their facility. (The 2025 Quality Awards program kicks off with the Nov. 14 Intent to Apply deadline, followed by the Jan. 23, 2025, application deadline):
Administrator, McMahon Tomlinson Nursing & Rehab
The process of participating in the AHCA/NCAL Quality Awards program was both rewarding and challenging for us.
Structuring the application to meet the rigorous criteria required a deep dive into our facility’s operations and quality initiatives. The team had to coordinate closely, refine our focus, and highlight measurable outcomes. Although challenging, the process motivated us to take a closer look at our systems, which, in itself, was beneficial for us.
We began by assembling a team that represented all aspects of our facility — from leadership and nursing to support staff and quality improvement. Each team member contributed data and insights specific to their area. We reviewed our performance metrics, resident satisfaction surveys, and past improvement projects. Additionally, we held brainstorming sessions to identify key successes and challenges, ensuring our application reflected a comprehensive view of our quality efforts.
Teamwork was essential in making this application successful. We established clear roles and a timeline, meeting regularly to discuss progress and address any challenges. Each department contributed information and reviewed drafts to ensure accuracy and consistency. This collaborative approach not only streamlined the application process but also strengthened our commitment to quality improvement as a united team.
Winning the Bronze Award has had a profound impact on our facility and staff. It boosted morale and reinforced a sense of pride in the care we provide. Staff members feel recognized and valued, and there’s a renewed motivation to maintain and exceed this standard. Our residents’ families and the local community have responded with positive feedback, often expressing appreciation for the dedication shown by our team. This award has increased our facility's visibility and reputation, reinforcing trust with current and prospective residents and their families.
Upon receiving the award, we displayed the award prominently within the facility and purchased a flag for our entrance.
To other CPO members considering the application, I’d say go for it! The application process can be challenging, but it’s a valuable opportunity for growth. Reflecting on your practices and outcomes offers insights that can lead to meaningful improvements, regardless of the award outcome.
Winning the Bronze Award not only recognized our efforts but also inspired us to strive for even higher standards. The award serves as a testament to the hard work of your team and communicates to your community that quality care is a priority.
SB 1511 also helps expand number of potential health care workers
By Tanecia Davis
Director Workforce Development

Tanecia Davis
Oklahomans with loved ones living in Long Term Care across our state can rest a little easier about the folks who are providing care inside those facilities for their family members.
Senate Bill 1511, authored by Sen. Jessica Garvin, passed both houses and signed by the Governor, amends existing state law and expands the categories of convicted felons that are ineligible to work for nursing homes, residential care and other Long Term Care facilities.
The legislation bars anyone convicted of a crime that results in that person being registered as a sex offender and those convicted of human trafficking offenses from working in Oklahoma Long Term Care.
Those new categories are in addition to the list of felonies that disqualify the person convicted from working in Long Term Care. Those include any convicted of abuse, neglect or financial exploitation of any person entrusted in their care; rape, incest or sodomy; child abuse; murder or attempted murder; manslaughter; kidnapping; aggravated assault and battery; assault and battery with a dangerous weapon or arson in the first degree.
As Care Providers Oklahoma's Director of Workforce Development and director of the Care Careers Oklahoma initiative working to grow the number of healthcare workers across the state, I'm glad to see the state taking action to protect our most vulnerable citizens.
I'm also happy to see that the legislation also provides an avenue for people convicted of non-violent felonies and misdemeanors to join the Long Term Care workforce quicker than under previous law.
SB 1511 lowers the elapsed time after completion of a sentence from 7 years to 5 for those convicted of lesser offenses.
I'm pretty sure that will have the effect to making more people eligible to work sooner in Long Term Care and help me in my job to build our workforce across the state.
Sen. Garvin shared her thoughts with me on the legislation and what it means to both the people living in Long Term Care and individuals who are eligible to resume their working lives a bit sooner than before.
"Senate Bill 1511 pairs common sense public policy with compassion for those who need a second chance at life," Sen. Garvin said. "This bill allows Long Term Care communities to connect with an untapped workforce by enabling non-violent offenders to get back to work sooner, which allows them to be more successful at avoiding re-entry.
"Long-term care facilities generally have close-knit staff who support one another through the ups and downs of life. I believe employing these individuals, and providing them with a network of coworkers who can offer encouragement, support, and friendship, will help these formerly incarcerated Oklahomans get back on their feet and back at life. In addition, it helps solve one of the major workforce issues we are having in this industry, and closer aligns our State's statutes with other surrounding states."
I call that common sense compassion.
Thank you, Sen. Garvin and all of our state legislators who supported this legislation.
Mandatory Off-cycle SNF Revalidation Process—What You Need to Know

Janine Lehman
By Janine Lehman, RN, RAC-CT, CLNC
Director of Legal Nurse Consulting, Proactive LTC Consulting
-
-
-
Major revision of SNF reporting on 855 – New SNF Disclosures Attachment
-
One-third of SNF providers will be notified in each month from Oct-Dec
-
-

Students participating in OIC of Oklahoma County at a recent meeting attended by CPO's Taneica Davis
Helping people discover healthcare opportunities by building trust and encouraging communication
By Tanecia Davis
Director of Workforce Development
I recently met with students working to obtain their GED through the Opportunities Industrialization Center (OIC) of Oklahoma County. I was there to help them discover their professional strengths.
Although some were initially hesitant, they later inquired about my work with individuals with felony records while I walked to my car. After learning about my experience, they shared more openly.
I've consistently observed that young adults require a caring and relatable approach to build trust and encourage open communication. It ended up being a great conversation!
It's great to see folks for whom life's circumstances have clouded their educational or career ambitions find their way to a brighter future.
That's why I'm so enthusiastic to offer free CNA training and job opportunities through Care Providers Oklahoma's Care Careers Oklahoma initiative.
Not only did I recently meet with the OIC students, but within the past couple of weeks I helped connect members of the current SidexSide OKC cohort with potential employment through CPO member Bridges Health.
Three Bridges Health facilities were among about a dozen Oklahoma employers who participated in a SidexSide OKC job fair at its downtown OKC offices.
The SidexSide job fair was a fast-paced event that provided candidates with the opportunity to engage in brief personalized interviews with prospective employers before moving on to the next participating employer.
If you are not familiar with SidexSide OKC, its primary objective is to provide individuals with the necessary resources and skills to secure sustainable employment.
The candidates are enrolled in a paid weekly cohort that focuses on developing their skills and preparing them for training and successful career placements.
We're happy to share this webinar presented by AHCA/NCAL and Incite Strategic Partners
The webinar features three Incite speakers who outline all that the Incite GPO offers members beyond just saving money. It is a great resource for CPO members who want to know more about the Incite GPO and how it works. The webinar also provides some great insight into Incite Strategic Partners. WATCH BELOW:
CPO's Natashia Mason outlines what is new in the upcoming changes to MDS

Natashia Mason
By Natashia Mason, RN, MSN
Director of Strategic Initiatives
Effective October 1, 2024 there will be a few minor changes (elimination of discharge goals to section GG) to the MDS as well as two new questions (tracking of Anticonvulsants and documentation of COVID vaccinations). These changes are outlined below.
Minor Changes
- Elimination of Section GG Discharge Goal
- MDS Coordinators will no longer need to document the Discharge goal on section GG, however, the functional status and goals still need to be added to the care plan.
- Coding guidelines changed for Septicemia on Item I2100 Septicemia. The RAI manual now states:
- “For sepsis to be considered septicemia, there needs to be inflammation due to sepsis and evidence of a microbial process." If the medical record does not reflect both items, then you enter the sepsis diagnosis and ICD code in item I8000. (Pg. I-15 RAI Manual)
- Considerations: Ensure documentation reflects the above information, if applicable, for septicemia.
Major Changes
- Documentation of COVID vaccination (O0350)
- The RAI manual now requires documentation of up-to-date COVID vaccination.
- The vaccination status may be determined from any available source, such as review of the resident’s medical record and/or interview with the resident, family, or other caregivers. If the resident is not up-to-date and the facility has the vaccine available, then it should be offered to the resident. (Pg. O-20 RAI Manual)
- Current definition of up to date should be referred to by using the CDC webpage.
- It is important that you refer to this definition for the ARD of the resident’s assessment, as this definition drives the decision when coding O0350. This question will be asked on all assessments, so ensure proper documentation in the resident’s record regarding COVID vaccination status.
- Considersations: Ensure the medical record and care plan reflects documentation of COVID vaccination status.
- Documentation of Anticonvulsants
- The MDS now requires documentation of Anticonvulsant medications and indication noted (N0415K1 and N0415K2). Remember, medications in section N0415 are coded according to the pharmacological classification not how it is used. If a medication is dually classified, then both classifications are coded in this section. (Pg. N-8 RAI Manual)
- Considerations: Ensure the care plan and documentation reflects the medication and indication for use.
The current RAI Manual effective October 1, 2024 can be found here.
If you have any questions, please don’t hesitate to reach out to Natashia via email at Natashia@careoklahoma.com
Care Providers Oklahoma Board Chair Tandie Hastings shares perspective on her bid for NCAL Board position

Tandie Hastings
By Tandie Hastings
CEO, Companion Health Services
The senior healthcare industry is in a constant state of evolution, with the needs of residents, their family members, and caregivers changing rapidly. For Care Providers Oklahoma (CPO), staying ahead of these shifts is vital to ensuring that our members are equipped to provide the highest quality of care. As we see a surge in the number of seniors needing assisted and nursing care, I want to lead our state association’s efforts to build a more impactful community of assisted living providers. That is why I am seeking a seat on the NCAL board of directors.
More than just an effort to apply my education and experience on a national level – I am seeking this office so that Care Providers Oklahoma and its members can enhance the services provided to assisted living providers and intensify our focus on building greater capacity for these communities.
I bring three decades of experience and a deep understanding of the challenges and opportunities within the assisted living sector. My position on the NCAL board would place care providers across Oklahoma in a unique position to influence national policy, share best practices, and stay ahead of industry trends. Here’s why my board seat is so critical for CPO members:
- Direct Representation at the National Level: My potential board position allows us to have a direct voice in discussions that shape the future of assisted living in the U.S. This means that the specific needs and challenges of Oklahoma's care providers will be represented in policy-making decisions that impact the entire country.
- Access to Resources and Information: Serving on the NCAL board would provide me access to cutting-edge research, trends, and resources that can be brought back to benefit CPO members. This includes insights on regulatory changes, innovative care models, and funding opportunities that can directly enhance the quality of care in Oklahoma.
- Networking and Collaboration: The NCAL board connects leaders from across the nation, fostering a collaborative environment where ideas and strategies are exchanged. My involvement opens opportunities for CPO members to engage with national leaders, participate in pilot programs, and collaborate on initiatives that drive improvements in assisted living.
As the population ages, the demand for assisted living services is increasing exponentially. Oklahoma, like many states, is seeing a growing need for high-quality assisted living facilities that can provide a continuum of care to an aging population. Here’s why CPO will prioritize its focus on assisted living members:
- Rising Demand for Assisted Living Services: With the aging Baby Boomer generation, there is a substantial increase in the number of older adults requiring assisted living services. CPO must ensure that our members are prepared to meet this demand with the highest standards of care.
- Regulatory Changes and Challenges: The assisted living sector is subject to evolving regulations that can be challenging to navigate. By focusing on these, CPO can provide the support, education, and advocacy necessary to help us comply with these regulations and continue delivering quality care.
- Diverse Needs of Assisted Living Residents: Residents in assisted living facilities have unique needs that differ from those in skilled nursing or independent living environments. CPO can play a crucial role in developing resources and training programs tailored to the specific challenges faced by assisted living providers, ensuring that they can offer personalized, compassionate care.
- Enhancing Quality and Innovation: By putting a focus on our assisted living members, CPO can drive innovation within the sector. Whether it’s through adopting new technologies, improving care coordination, or implementing quality improvement initiatives, a dedicated focus on assisted living will help Oklahoma’s care providers stay ahead of the curve.
If I am successful in my candidacy for the NCAL board, our association will be positioned to make a meaningful impact at the national level. This role not only brings valuable insights and resources to our state but also underscores the importance of focusing on the assisted living sector. As we move forward, prioritizing the needs of our assisted living members will be essential to ensuring that we continue to provide the highest quality of care to our aging population. Together, with strong leadership and a commitment to excellence, CPO and its members can navigate the challenges ahead and thrive in the ever-changing landscape of senior healthcare.

A member of the SidexSide job skills cohort meets with the team from Voyage Long Term Care at Job Fair.
SidexSide OKC brings skills training and employment opportunities to underemployed Oklahomans
Editor's Note: Tanecia Davis is CPO's Director of Workforce Development and manages our Care Careers Oklahoma workforce development program
By Tanecia Davis
Director of Workforce Development
I recently had the pleasure of visiting SidexSide OKC for their career fair, and I was thoroughly impressed by the exceptional work they are doing to support underemployed individuals.
I was there to support CPO member Voyage Long Term Care, which participated in the Job Fair as one of several health care employers.
SidexSide's primary objective is to help these individuals with the necessary resources and skills to secure sustainable employment.
The candidates are enrolled in a paid weekly cohort that focuses on developing their skills and preparing them for training and successful career placements.
The career fair was structured as a speed dating-style event, providing candidates with the opportunity to engage in brief personalized interviews with prospective employers. Every candidate was dressed professional and demonstrated the tools they learned throughout the cohort. Every employer spoke nothing but great things about the organization and cohort!
If you know anyone who could benefit from SidexSide OKC's programs, please connect them with the organization for their upcoming cohort. SidexSide
I wasn't the only one impressed by the SidexSide mission. Here is what Sarah Bussey, Voyage Long Term Care's Human Resources Director, posted on LinkedIn in the wake of the Job Fair:
"We had such a wonderful time at SidexSide’s debut of Care Careers Oklahoma! We plan to come back each month, wonderful people, excellent candidates, overall a wonderful display of community and leadership. Thank you for having us!"
More perspective: Here's what Jim Stafford, CPO's Content Creator, wrote in his personal blog about SidexSide. Jim stopped by the SidexSide job fair to take some photos of the Voyage team meeting with potential employees.
I'm glad a CPO member like Voyage was able to participate in this worthy event.

Aerial view of Barnsdall in aftermath of spring tornado
Employees of 3 Oklahoma Long Term Care Facilities receive funds to help with repairs, replacement
In the wake of an outbreak of violent Spring tornadoes across Oklahoma, Care Providers Oklahoma's Helping Hands fund has stepped in to provide financial assistance to employees at member facilities who suffered loss or damage to personal property.
As of the first week of July, our Helping Hands fund had provided $3,000 to seven employees from three facilities in Barnsdall and Ardmore. The funds will help employees replaced damaged vehicles, roofing and broken window repair, mending fences and even with costs of relocating because their home was destroyed.
"We're so grateful to have this fund available and to be able to provide meaningful aid to these employees whose lives were disrupted by the tornadoes, said Steven Buck, CPO President/CEO. "When you see us raising money through our 50-50 jackpot at the Spring and Fall conventions, remember that devastation like these tornadoes caused are the reason for the fund."
The Helping Hands fund provides assistance to employees facing financial challenges because of the loss of property, but also was used to provide food to staff members of nursing facilities that accepted emergency transfer of residents from storm damaged nursing homes.
Here's a brief recap of how the tornadoes impacted member facilities across the state this past Spring:
Tornadoes swept through Marietta, Sulphur and Holdenville on April 30, destroying much of those communities and heavily damaging the Lake Country Nursing Center in Marietta.
Less than a week later, an F4 tornado devastated the Northeast Oklahoma community of Barnsdall, destroying many of the buildings in town and damaging others, including the Barnsdall Nursing Home.
The Barnsdall Nursing Home was damaged when it struck by debris and a large tree fell into it, forcing evacuation of all 30 residents. No injuries were reported at the nursing home.
Residents were moved to other nursing homes in the area, including Nowata and Claremore.
The Skiatook Nursing Home also suffered damage during the storm, but no residents were injured or evacuated.
Other facilities suffering damage included the Colonial Terrace Care Center and Shady Rest Care Center, both in Prior.
The Barnsdall tornado came on the heels of another devastating twister that devastated Marietta, Sulphur and Holdenville the previous week, claiming four lives.
The Lake Country Nursing Center was heavily damaged when the F4 tornado struck Marietta. Nursing Center staff evacuated all 60 residents, and while minor injuries were reported, there were no deaths.
Take important steps to show that you value employees well being and development
By Tanecia Davis
Director of Workforce Development
 There is more to our Care Careers Initiative than connecting potential new employees with training and jobs. We also are focused on employee retention and keeping the folks you've invested as employees for the long term.
There is more to our Care Careers Initiative than connecting potential new employees with training and jobs. We also are focused on employee retention and keeping the folks you've invested as employees for the long term.
I recently saw this article from HealthLeadersMedia.com that emphasized the importance of employee satisfaction and happiness to building a long term staff.
Here's a paragraph that makes that point:
"Though the strength of a workforce is still very much measured in numbers such as costs and turnover rate, prioritizing less easily quantifiable areas like employee satisfaction and happiness has the potential to result in a more sustainable workplace model."
The bottom line? Taking steps to initiate programs that place value on employee well being, professionalism and development can create a more sustainable workforce for Oklahoma LTC providers.
If you are looking to build your facility's workforce or want to take your first steps into a health care career, attend our next Career Fair on July 24 at the McKeon Creativity Center, 910 South Boston Ave., in downtown Tulsa.
One more paragraph from the Health Leaders Media article:
"The proof is undeniable: Cultivate a positive environment for your workforce and the results will follow."

Barnsdall Nursing Home after tornado struck in early May. (photo by Ben Abrams/KWGS News)
Tornadoes damage member facilities, force evacuations in Marietta, Barnsdall
By Jim Stafford
Content Creator
When tornadoes rolled across several Oklahoma communities this past April and May, several Care Providers Oklahoma member facilities suffered damage, impacting both residents and their staffs.
Our Helping Hands fund was created for just these types of situations.
The Helping Hands fund aids employees facing financial challenges because of the loss of property, but also has been used this spring to provide food to staff members of nursing facilities that accepted emergency transfer of residents from other storm damaged nursing homes.
Here's a recap of what happened when violent weather struck across the state in late April and early May and how it impacted our member facilities and their residents:
Tornadoes swept through Marietta, Sulphur and Holdenville on April 30, destroying much of those communities and heavily damaging the Lake Country Nursing Center in Marietta.
Less than a week later, an F4 tornado devastated the Northeast Oklahoma community of Barnsdall, destroying many of the buildings in town and damaging others.
The Barnsdall Nursing Home was damaged when it struck by debris and a large tree fell into it, forcing evacuation of all 30 residents. No injuries were reported at the nursing home, although one Barnsdall resident died in the storm.
“The damage done here was substantial to the roof, and obviously with the rain, they’ve got a lot of damage inside,” Barnsdall Mayor Johnny Kelley said of the nursing home damage.
Residents were moved to other nursing homes in the area, including Nowata and Claremore.
Many other facilities received minor damage in the storms.
The Barnsdall tornado came on the heels of another twister that devastated Marietta, Sulphur and Holdenville the previous week, claiming four lives.
The Lake Country Nursing Center in Marietta was heavily damaged when an F4 tornado struck that community. Nursing Center staff evacuated all 60 residents, and while minor injuries were reported, there were no deaths.
“God just spread his wings over that facility,” operator Tom Coble said.
So, how is CPO and our Helping Hands fund providing assistance through all of this?
Through our Helping Hands fund, we’ve provided meals to the staffs at Emerald Care Center in Claremore and Nowata Nursing Center, both of which accepted residents impacted by the storm in Skiatook.
We’re still gathering information on potential personal property damage to employees at any of our member facilities impacted by the storms. The Helping Hands fund will be there to help.
"When you see us raising money through our 50-50 jackpot at the Spring and Fall conventions, remember that devastating situations like these tornadoes caused are the reason for the fund," said Steven Buck, CPO President/CEO. “A special thanks to AHCA/NCAL state affiliates for pitching in, as well as many individuals.
"Your generosity can mean so much to our heroic staffs who ensured our vulnerable residents were sheltered during the storms despite knowing there was possibility of their own residences and families being adversely impacted."
Oklahoma’s Josh Wood of Bridges Health Selected for National “Future Leaders” Program

Josh Wood
OKLAHOMA CITY – Care Providers Oklahoma is proud to announce that Josh Wood (photo attached) of Bridges Health has been selected by the American Health Care Association/ National Center for Assisted Living (AHCA/NCAL) as a future leader in long term and post-acute care. Wood will participate in AHCA/NCAL’s Future Leaders program, which provides year-long training and mentorship for professionals in long term and post-acute care.
Bridges Health is an employee-owned Skilled Nursing & Therapy Facility Management Company operating exclusively in Oklahoma. Wood has served as a regional manager at Bridges since 2020.

May 30, 2024
For Immediate Release
Media Contacts:
Alex Weintz; Aweintz@amberintegrated.com; 914-282-3229
Lawmakers approve $30 million in new funding for Oklahoma's nursing homes and facilities caring for individuals with developmental disabilities
"In the next legislative session, our goal will be to increase funding to a level that meets the actual cost of care for our Medicaid recipients. Getting to that level is the only way to guarantee that Oklahoma has stable, high quality skilled nursing and longterm care providers that can serve our most vulnerable loved ones and neighbors." -- Care Providers Oklahoma President and CEO Steven Buck

Poodle skirts and rolled up jeans will be in fashion at the Sock Hop during CPO's Spring Convention
By Jim Stafford
CPO Content Creator
There was a scene in the 1984 movie Sixteen Candles where a group of nerdy young men attend a school dance, lined up against a wall watching the girls, but too intimidated to ask any of them to dance.
That was me in the 1960s at any activity that included girls and dancing, My fellow nerds and I wiled away the time while talking a big game but never leaving the wall we were leaned up against.
I've written this because Care Providers Oklahoma has scheduled its own version of the 1960s Sock Hop at its annual Spring Convention and Trade Show April 30-May 2.
Our throwback "Twist and Shout" event, sponsored by PharmcareUSA/Oklahoma, will occur from 8-10 pm on May 1 at the Embassy Suites & Convention Center in Norman. It's all part of the Music of the Decades theme of the Convention and all of our major events this year. Register!
We're going to be all poodle skirts and rolled up jeans (someone get me a pack of Luckies!) at the Sock Hop, and encourage participants attending the Convention to dress the same, although it's not required.
We are going to have a costume contest, dance contest, bubble gum blowing contest, and hula hoop contest as well, at the Wednesday night Sock Hop. There will be prizes!
And if you're distracted by the OKC Thunder playoff game that night, we'll have it showing on the big screen, too.
As to the music, a special DJ will be spinning the tunes from the '50s through the '80s, so feel free to request your favorite. Then grab a partner and get out there on the dance floor.
Of course, I'll be watching from the nerd section and feeling some '60s nostalgia creeping up on me. And not making any eye contact with the girls in poodle skirts and bouffant hairdos.
That's a memory that hits a little too close to home.
BONUS: We've also scheduled a special Music Trivia contest from 5:15-6:30 pm on April 30 in the bar area of the Embassy Suites. Come test your knowledge of popular music across the decades of the '50s through the '80s. Did I mention there will be prizes?


Sarah Becker, RN
By Sarah Becker, RN, RAC-CT, DNS-CT, QCP
Start Early: Waiting until the survey concludes and the CMS-2567 form arrives is not advisable. Begin drafting the PoC on the day of exit, using insights from the exit conference. In addition, the facility team should promptly initiate needed corrective actions.
Addressing Deficiencies: When responding to deficiencies, consider the following elements:
Regulatory Reference: The CMS-2567 will include the survey data tag number, relevant CFR (Code of Federal Regulation) or LSC (Life Safety Code) reference, and language specifying the noncompliant aspect. Your plan of correction must address how you are correcting your non-compliance with that specific regulatory requirement.
Deficient Practice Statement: The CMS-2567 will describe specific actions, errors, or lack of action constituting the deficient practice. Each of these elements should be addressed through your corrective action plan.
Submission Timeline: After the survey exit, the facility should receive the Form CMS-2567 Statement of Deficiencies within 10 business days (via email). Within 10 calendar days of receipt, an acceptable PoC must be submitted to the Survey Agency. This requirement applies to deficiencies falling within scope and severity Levels B through L.
Analyze the Statement of Deficiencies:
Plan of Correction Requirements
The plan of correction will serve as the facility’s allegation of compliance. SOM Chapter 7 – 7317 Acceptable Plan of Correction

A prospective employee meets reps from a nursing facility at our Fall 2023 Job Fair
By Tanecia Davis
Workforce Ambassador
Care Careers Oklahoma is hosting a Job Fair April 10 at Metro Tech's Springlake campus with a goal to connect those interested in learning about Long Term Care employment with training and job opportunities.
Our Job Fair is a casual, come-and-go event from 9 am to 2 pm in which you are invited to wander among the information tables, meet with the reps from 11 Oklahoma facilities and explore the career possibilities.
So, why are we doing this? Just look at the employment numbers recently reported by the American Health Care Association/National Centers for Assisted Living, the partner organization with Care Providers Oklahoma:
According to AHCA/NCAL's 2024 State of the Sector Report, 99% of all nursing homes are currently hiring.
Ninety-nine percent!
And 90% have increased wages as they work to fill positions.
Here in Oklahoma, nursing home employment tracks along those trends with a virtual 'help wanted' sign posted at almost every facility across the state.
Care Providers Oklahoma, through its Care Careers Oklahoma initiative, is committed to helping increase the pool of trained workers who can fill those positions.
So, the Job Fair is one of those steps.
As CPO's Workforce Ambassador and director of the Care Careers program, and I would love to meet you at the Job Fair and discuss the CMA and CNA training process. You may discover that your passion is leading you down this career path.
The jobs are waiting to be filled.


ICF Day at the Capitol brought residents, staff and displays to the second floor Rotunda.
By Jim Stafford
CPO Content Creator
CPO ICF Day at the Capitol brought smiles and joy to the second floor Rotunda at the State Capitol this week with the presence of more than 100 residents, staff and parents from Oklahoma Intermediate Care Facilities for Individuals with Intellectual Disability (ICF/IID).
My job with Care Providers Oklahoma brought me to the Capitol to capture some of the ICF Day activities in photos and video.
So, I was milling around the Rotunda when I spotted a tall, slender man with flowing gray hair being interviewed by a local television station.

Rick Bozarth, a parent of an ICF resident, shares his perspective during an interview on ICF Day at the Capitol.
When the interview ended, I walked up and introduced myself as a CPO employee. Turns out, the man was Rick Bozarth of Seiling, a parent of an adult child who lives in an Enid facility operated by Oklahoma Homes for the Developmentally Disabled.
Bozarth is an attorney and former District Judge who described the Enid facility as a "godsend" for his son -- and his son’s parents, as well.
"It's a wonderful operation," Bozarth told me. "To be able to sleep at night is worth it, to have your kids be protected, especially if your kid is disabled. So many people don't have a clue as to what that's like, to have to deal with those issues with your child all year long."
For Bozarth, that means knowing that his adult son lives in a safe environment that has 24-7 care.
"These people give you peace of mind," he said.
About 1,800-2,000 people reside in ICF homes across Oklahoma, said Justin McGrew, an ICF operator who was one of three CPO Board Members who served as an advisory group for ICF Day activities.
McGrew said the purpose of the day was to generate attention of ICF homes with legislators as operators seek the maximum reimbursement rate allowed by CMS for residents in their care.
"We're trying to create some awareness of our populations," McGrew said. "As an example, we are getting paid $50 a day less than nursing homes, but large IID centers with a heavy level of care and 24-hour nursing ... it's hard to keep up and not get paid close to some of the other providers. A lot of times we get lost."
ICF Day activities included informational tables and booths set up in the Rotunda, visits to offices of individual legislators, interviews with local media, a luncheon that featured short addresses from three legislators, and opportunity to watch floor debate from the House and Senate galleries.
I sat in the Senate gallery next to Michelle Devauld of Oklahoma City, whose adult son lives at the Billings Fairchild Center. Her son has lived there for 14 years.

Michelle Devauld (waving) among onlookers in the Senate Gallery on ICF Day at the Capitol.
"I've got to tell you that it was the hardest choice to let go of the reins and let him live somewhere by himself," Michelle told me as we waited for the afternoon Senate session to begin. "But I know at night he is very well taken care of with 24-hour nurses there. The staff is great, the caregivers all the way down to the janitor."
Plus, there are learning and social opportunities.
"He's doing things he's never done before, had he lived with my husband and I," Michelle said. "He has a roommate. He is very independent. He goes to classes. He learns things that you and I take for granted, like tying his shoes, hygiene, matching colors, counting money, sorting and putting silverware in a napkin, rolling it up and putting it on a table."
"I don't have any complaints whatsoever," she said. "I'm happy that he's there."

Journal Record photo

Courtney Bishnoi
By Courtney Bishnoi
Did you know that OSHA recently expanded its record keeping requirements? Nearly all providers are already required to maintain OSHA 300 Logs, Form 301, and Form 300A and submit 300A summary data before March 2nd each year. The NEW requirement for employers with 100 or more employees adds additional information to be submitted: OSHA 300 logs and Form 301 (incident reports).
By Jim Stafford
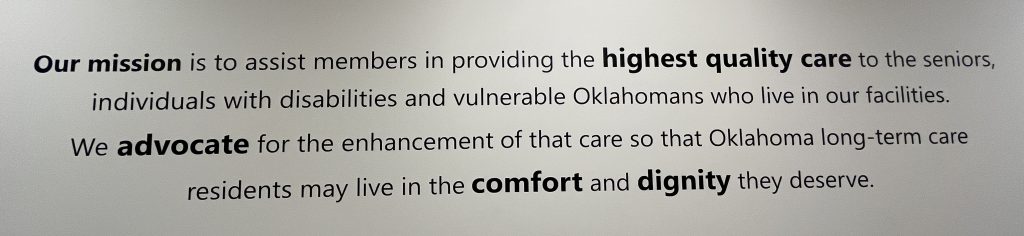
CPO Content Creator I was struck by the sudden appearance of the Care Providers Oklahoma mission statement on the wall as I entered the CPO offices for the first time after the holidays.
There, in large black letters along the wall on the left side of the foyer as you walk to our classroom space, are these words:
"Our mission is to assist members in providing the highest quality care to the seniors, individuals with disabilities and vulnerable Oklahomans who live in our facilities. We advocate for the enhancement of that care so that Oklahoma long-term care residents may live in the comfort and dignity they deserve."
Then, when you have it crafted the way you want it, it's added to your website, perhaps, and promptly forgotten about by most employees, and rarely seen by the public.
I asked Steven Buck, CPO President/CEO, why our mission statement was given so prominent a space. Here's what he told me:
"For the past three plus years, the pandemic has been the predominant story in service to our members. As we continue to emerge from the worst days of the pandemic I wanted to emphasize the importance of all aspects of the association's business to center on serving our members and, through their excellence, benefitting Oklahoma's seniors and most vulnerable."
That's a compelling reason for making the mission statement so, well, obvious, in its new space for me and my colleagues here at CPO.

Shelly Maffia
By Shelly Maffia, RN, MSN, MBA, LNHA
Immediate Jeopardy Citations signify situations where a nursing facility’s non-compliance poses substantial risk to residents’ health and safety. Understanding causative factors behind these citations plays a pivotal role in driving continuous improvement in nursing facility care.
|
Top Five IJ Citations
|
# IJ Citations
|
% Providers Cited
|
% Surveys Cited
|
|
1. F689 – Free of Accident Hazards/Supervision/Devices
|
864
|
4.7%
|
38.8%
|
|
F689 citations arise when facilities fail to provide adequate supervision, resulting in accident hazards for residents. This underscores the importance of robust safety measures and vigilant supervision to prevent incidents that could harm residents. The most common situations resulting in F689 IJ citations include elopements, accidents involving mechanical lifts, transportation accidents, and incidents involving smoking or choking.
|
|||
|
2. F600 – Free from Abuse and Neglect
|
525
|
2.8%
|
23.6%
|
|
F600 was the second most frequently cited Immediate Jeopardy area in FY2023, which emphasizes the critical need for nursing facilities to create an environment free from abuse and neglect. Ensuring staff awareness, proper training, and implementing stringent anti-abuse policies are vital steps in avoiding this citation.
|
|||
|
3. F684 – Quality of Care
|
268
|
1.5%
|
12.0%
|
|
Quality of care is at the heart of nursing facility services. Immediate Jeopardy in this category highlights deficiencies that directly impact residents’ health and well-being. Maintaining high-quality care involves continuous evaluation, staff training, and adherence to best practices.
|
|||
|
4. F835 – Administration
|
183
|
1.0%
|
8.2%
|
|
Administrative lapses can lead to Immediate Jeopardy situations. Facilities must ensure efficient administration, including proper documentation, adherence to regulations, and effective communication channels within the organization.
|
|||
|
5. F880 – Infection Control
|
154
|
0.8%
|
6.9%
|
|
Infection control is a critical area for nursing facilities. Immediate Jeopardy arises when facilities fail to implement robust infection control measures, putting residents at risk. Strict adherence to infection prevention protocols is paramount.
|
|||

Kenn Daily
By Kenn Daily
For more than 5 years I have been teaching a two-day Life Safety Code compliance workshop for Maintenance Supervisors, Facility Managers and Administrators. Well, last Monday I was traveling to Tulsa, Oklahoma, to teach a boot camp for Care Providers Oklahoma.
I headed to the airport for my 7:15 pm flight, arriving early and having plenty of time to get through TSA and to the gate.
Arriving at the gate I received a notice from the airline that my flight would be leaving about a half-hour late, but that was fine because I had more than an hour layover scheduled. Then an announcement was made that the flight would be leaving more than an hour and a half late due to no crew and then a few minutes after that the flight would be canceled, ironically for no staff.
At this point, I would miss my connection and never make it to Tulsa that evening. So, I called the airline customer service who was pleasant and tried to be helpful but could only get me on an afternoon flight for the next day getting me in to Tulsa at 5 pm.
This was a whole day later than planned and would shorten my boot camp to a single day.
In the end, what I learned was many industries, not just senior living, are suffering from low or no staff to meet their customer’s needs.
EDITOR’S NOTE: Kenn, we’re so glad you finally made it safely to Tulsa and met the challenge of providing two days of Life Safety education into a single-day class.

Christine Twombly
Earlier this year CMS transitioned from QIES to IQIES for MDS submission and CASPER reporting access. This transition left some MDS coordinators confused about how to access reports that were previously made available through QIES.

Brandy Hayes
By Brandy Hayes, RN
Clinical Consultant, Proactive LTC Consulting
-
Education: Staff should be well-versed in proper medication administration techniques and the adverse effects of medications. This knowledge equips them to be observant and proactive in recognizing adverse effects of medications promptly.
-
System Implementation: Establish a systematic approach to ensure that each resident’s medication usage is evaluated upon admission and on an ongoing basis. This system should identify risks and problems and take appropriate actions. Use the critical element pathway 20082 Unnecessary Medications to guide QA efforts.
-
Medication Reconciliation (N2001): “Clinically significant medication issue is a potential or actual issue that, in the clinician’s professional judgment, warrants physician (or physician-designee) communication and completion of prescribed/recommended actions by midnight of the next calendar day at the latest. ‘Clinically significant’ means effects, results, or consequences that materially affect or are likely to affect an individual’s mental, physical, or psychosocial well-being, either positively, by preventing a condition or reducing a risk, or negatively, by exacerbating, causing, or contributing to a symptom, illness, or decline in status. Any circumstance that does not require this immediate attention is not considered a potential or actual clinically significant medication issue for the purpose of the drug regimen review items.”
-
Medication Follow-up (N02003): The process of contacting a physician to communicate an identified medication issue and completing all physician- prescribed/recommended actions by midnight of the next calendar day at the latest.
-
Medication Intervention (N02005): Every time a potential or actual clinically significant medication issue is identified throughout the resident’s stay, it must be communicated to a physician, and the physician-prescribed/-recommended actions must be completed by the clinician in a time frame that maximizes the reduction in risk for medication errors and resident harm.

Champions of Health Awards Presentations were held in massive ballroom at the OKC Convention Center
By Jim Stafford
CPO Content Creator
I was privileged to be part of the Care Providers Oklahoma team that attended the 2023 Champions of Care Awards Presentations recently at the OKC Convention Center.
The Champions of Health awards program was launched in 2004 to recognized organizations and individuals working to improve health outcomes across Oklahoma. Proceeds from the Awards Presentations ceremony benefits the Oklahoma Caring Foundation, a not-for-profit that provides preventative health services to underserved Oklahomans.
The Champions of Health Awards were presented by Blue Cross and Blue Shield of Oklahoma.
CPO is one of 11 member organizations that comprise the Champions of Health Coalition Partners, and Steven Buck, CPO President/CEO is part of the Coalition Leadership team.
"Champions of Health is a celebration of innovation in health delivery to vulnerable populations in our state,” Steve said. “I have been involved in Champions for over 15 years and am always amazed by the quality of emerging approaches to providing care. It is an honor to stand with colleague organizations like Oklahoma Hospital Association and the Oklahoma State Medical Association to showcase these accomplishments."
Awards were presented in five categories to organizations that are pursuing innovative health related programs that can be replicated in other communities. Several CPO team members, including me, were among the judges who helped determine this year's winners.
Recipients recognized at the ceremony were:
Tulsa Public Schools as Champion of Children's Health for its student wellness progam.
Calm Waters as Champion of Senior Health for its grief support groups that are offered to seniors 55-plus who have experienced loss of a loved one.
Grand Mental Health as Champion of the Uninsured for providing health care services to under insured/uninsured Oklahomans.
Tulsa CARES as Champion of Community Health for being a provider of prevention and care programs for low income individuals living with HIV or Hepatitis C.
Neighborhood Services Organization as the Dr. Rodney L. Huey Memorial Champion of Oklahoma Health for its program to provide transitional and permanent housing for the unhoused to build stability, security and restore health.

NFL star Damar Hamlin participated in a fireside chat with Robin Marsh at the Champions of Health Awards Presentations
There were probably 1,000 folks or more at the Champions of Health Awards Presentation, and I'm sure that for some (me included) the big draw was the presence of NFL star Damar Hamlin, a defensive back with the Buffalo Bills.
If you're not familiar with Damar, he was the young man who collapsed on the field last January after a hard tackle. His heart stopped and it took heroic efforts by the team's training staff and medical personnel to revive him before transporting him to the hospital, where he spent 9 days.
Hamlin eventually was cleared to resume his NFL career and played in his first game of the 2023 season this past weekend.
In his OKC appearance, Damar participated in a 'fireside chat' facilitated by TV news personality Robin Marsh. He spoke about his past and the hard work it took to become an NFL player, and then his new mission of ensuring emergency technology like that which saved his own life is available to teams and organizations nationwide.
"‘It’s kind of like a calling, and we don’t get to choose our calling." he told the audience.
It was a touching presentation that showed a side of a professional athlete that we rarely get to see. For more on Damar's brush with death and his chat with Robin Marsh, read the post I wrote at Jim Stafford's BlogOKC.
Damar's presentation capped an important evening to organizations like CPO and our counterparts who support better health outcomes for all Oklahomans.
I'm glad I attended.

My CPO colleagues and I took a selfie outside the OKC Convention Center with Champions of Health emcee Robin Marsh
BONUS! My CPO colleagues -- Tanecia Davis, Juliet Williams and Shanna Reece -- and I happened to come across Robin Marsh just outside the convention center as we were leaving after the presentations concluded, and someone asked Robin if she would do a group 'selfie' with us.
Of course, she gladly accommodated us, and the result is the souvenir photo to the left.
 By Eleisha Wilkes, RN
By Eleisha Wilkes, RN
Connie Guinn
By Connie Guinn
Director of Education, Care Providers Oklahoma
When CMS adopted the 2012 Life Safety Code and the Healthcare Facilities Code more than three years ago, it created new expectations for inspection, testing and maintenance of fire protection features in long term care facilities.
So, Care Providers Oklahoma is offering an intensive 2-day training on Dec. 5 & 6 especially for facility and maintenance managers, environmental services directors, administrators and long term care safety consultants.
The class will be held on the OSU/Tulsa campus and led by Kenn Daily, LNHA, president of Ohio-based Elder Care Systems Group. Kenn presents the training under the title, "Don't Get Burned: Your Next Life Safety Code Survey.”
The training focuses on the requirements of NFPA 101 Life Safety Code and NFPA 99 Healthcare Facilities Code and the tightening of requirements through stricter implementation that their adoption by CMS brought.
"This is Life Safety Code training for skilled nursing facilities, with a comprehensive review of the current Life Safety Code requirements, as well as a discussion of step-by-step ways to Life Safety Code compliance, the most common deficiencies, and ways a facility can identify and correct items in advance," Kenn said.
The Life Safety Code established minimum criteria for many protective features and systems, including fire protection, generators, doors, building services and maintenance activities.
Under Kenn's leadership, our unique Boot Camp helps you understand practical applications of the Life Safety Code and learn from a life safety expert on what to prepare for during survey. The comprehensive program examines all sections of the LSC applicable to skilled nursing and providers formers, policies and best practice guides for use by healthcare organizations.
"Life Safety Code Compliance and preparation are critical for skilled nursing, and I'll highlight some lessons learned from other facilities across the country and some of the missteps facilities have experience and ways that you all can be better compliant," he said.
Here's a sample of some of the topics covered: LSC origins and organization; construction types, operating features, door locks, hazardous areas, fire protection systems, smoke compartments, fire barriers, building services and many others.
We hope to see you there.
Registration closes at 11 pm, Sunday, Dec. 3. Register here.

Christine Twombly
Earlier this year CMS transitioned from QIES to IQIES for MDS submission and CASPER reporting access. This transition left some MDS coordinators confused about how to access reports that were previously made available through QIES.

Brandy Hayes
By Brandy Hayes, RN
Clinical Consultant, Proactive LTC Consulting
-
Education: Staff should be well-versed in proper medication administration techniques and the adverse effects of medications. This knowledge equips them to be observant and proactive in recognizing adverse effects of medications promptly.
-
System Implementation: Establish a systematic approach to ensure that each resident’s medication usage is evaluated upon admission and on an ongoing basis. This system should identify risks and problems and take appropriate actions. Use the critical element pathway 20082 Unnecessary Medications to guide QA efforts.
-
Medication Reconciliation (N2001): “Clinically significant medication issue is a potential or actual issue that, in the clinician’s professional judgment, warrants physician (or physician-designee) communication and completion of prescribed/recommended actions by midnight of the next calendar day at the latest. ‘Clinically significant’ means effects, results, or consequences that materially affect or are likely to affect an individual’s mental, physical, or psychosocial well-being, either positively, by preventing a condition or reducing a risk, or negatively, by exacerbating, causing, or contributing to a symptom, illness, or decline in status. Any circumstance that does not require this immediate attention is not considered a potential or actual clinically significant medication issue for the purpose of the drug regimen review items.”
-
Medication Follow-up (N02003): The process of contacting a physician to communicate an identified medication issue and completing all physician- prescribed/recommended actions by midnight of the next calendar day at the latest.
-
Medication Intervention (N02005): Every time a potential or actual clinically significant medication issue is identified throughout the resident’s stay, it must be communicated to a physician, and the physician-prescribed/-recommended actions must be completed by the clinician in a time frame that maximizes the reduction in risk for medication errors and resident harm.

Champions of Health Awards Presentations were held in massive ballroom at the OKC Convention Center
By Jim Stafford
CPO Content Creator
I was privileged to be part of the Care Providers Oklahoma team that attended the 2023 Champions of Care Awards Presentations recently at the OKC Convention Center.
The Champions of Health awards program was launched in 2004 to recognized organizations and individuals working to improve health outcomes across Oklahoma. Proceeds from the Awards Presentations ceremony benefits the Oklahoma Caring Foundation, a not-for-profit that provides preventative health services to underserved Oklahomans.
The Champions of Health Awards were presented by Blue Cross and Blue Shield of Oklahoma.
CPO is one of 11 member organizations that comprise the Champions of Health Coalition Partners, and Steven Buck, CPO President/CEO is part of the Coalition Leadership team.
"Champions of Health is a celebration of innovation in health delivery to vulnerable populations in our state,” Steve said. “I have been involved in Champions for over 15 years and am always amazed by the quality of emerging approaches to providing care. It is an honor to stand with colleague organizations like Oklahoma Hospital Association and the Oklahoma State Medical Association to showcase these accomplishments."
Awards were presented in five categories to organizations that are pursuing innovative health related programs that can be replicated in other communities. Several CPO team members, including me, were among the judges who helped determine this year's winners.
Recipients recognized at the ceremony were:
Tulsa Public Schools as Champion of Children's Health for its student wellness progam.
Calm Waters as Champion of Senior Health for its grief support groups that are offered to seniors 55-plus who have experienced loss of a loved one.
Grand Mental Health as Champion of the Uninsured for providing health care services to under insured/uninsured Oklahomans.
Tulsa CARES as Champion of Community Health for being a provider of prevention and care programs for low income individuals living with HIV or Hepatitis C.
Neighborhood Services Organization as the Dr. Rodney L. Huey Memorial Champion of Oklahoma Health for its program to provide transitional and permanent housing for the unhoused to build stability, security and restore health.

NFL star Damar Hamlin participated in a fireside chat with Robin Marsh at the Champions of Health Awards Presentations
There were probably 1,000 folks or more at the Champions of Health Awards Presentation, and I'm sure that for some (me included) the big draw was the presence of NFL star Damar Hamlin, a defensive back with the Buffalo Bills.
If you're not familiar with Damar, he was the young man who collapsed on the field last January after a hard tackle. His heart stopped and it took heroic efforts by the team's training staff and medical personnel to revive him before transporting him to the hospital, where he spent 9 days.
Hamlin eventually was cleared to resume his NFL career and played in his first game of the 2023 season this past weekend.
In his OKC appearance, Damar participated in a 'fireside chat' facilitated by TV news personality Robin Marsh. He spoke about his past and the hard work it took to become an NFL player, and then his new mission of ensuring emergency technology like that which saved his own life is available to teams and organizations nationwide.
"‘It’s kind of like a calling, and we don’t get to choose our calling." he told the audience.
It was a touching presentation that showed a side of a professional athlete that we rarely get to see. For more on Damar's brush with death and his chat with Robin Marsh, read the post I wrote at Jim Stafford's BlogOKC.
Damar's presentation capped an important evening to organizations like CPO and our counterparts who support better health outcomes for all Oklahomans.
I'm glad I attended.

My CPO colleagues and I took a selfie outside the OKC Convention Center with Champions of Health emcee Robin Marsh
BONUS! My CPO colleagues -- Tanecia Davis, Juliet Williams and Shanna Reece -- and I happened to come across Robin Marsh just outside the convention center as we were leaving after the presentations concluded, and someone asked Robin if she would do a group 'selfie' with us.
Of course, she gladly accommodated us, and the result is the souvenir photo to the left.
 By Eleisha Wilkes, RN
By Eleisha Wilkes, RNBy Linda Farrar, RN

Do you ever feel like you are on an island and no one else knows or cares what you are going through in your long term care profession?
CPO provides educational opportunities, both virtually and in person all
year long through webinars and through in-person attendance at specific trainings, convention, Fall Fair and the Leadership Conference.
They are wonderful learning and networking opportunities, but the providers reported they wanted something closer to home so more staff could attend, smaller venues so sharing could be more comfortable, and still able to offer CEUs for a reasonable price.
Ta-Da!
Thus came the CPO Road Shows.
The agenda is planned completely based on the needs and wants of the providers. In our last trip, we spent the morning session talking about survey trends, and digging deeper into the tag numbers to talk about specific findings and apparent expectations of surveyors. During this session, attendees can share their own experiences. And believe me, there is plenty of “venting” going on also, which we all need sometimes. We also try to provide some tools and resources for facility use as appropriate.
Also discussed in this last trip included: Advance Directives: the expectations, evidence-based best practices, and tools, including INTERACT 4.0 and other tools; the need and importance of appropriate
Scheduled Drug Reconciliation; and expectations for a thorough and complete ANE investigation.
I would be remiss if there was no discussion about the sponsorship of PharmCare. WHAT A TEAM OF EXPERTS! They provided the venues in all three locations along with meals and snacks in all three locations. But as important, they shared experiences from their practices and their expertise.
The subject matter of the next Road Trip, which is scheduled for October 24, 25 and 26 with locations yet to be determined, is whatever you want it to be. Discussion of survey trends and findings will likely be included. Beyond that, what information would you like to have or discuss? It is an honor and a pleasure for me to be working in Oklahoma.
We are here to help … just tell us how.



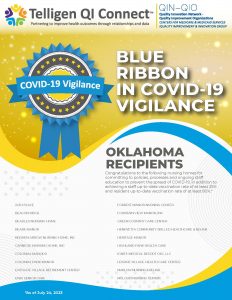



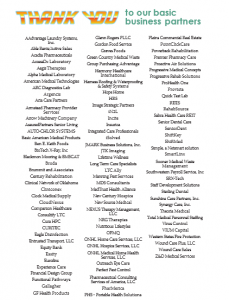





 With this year’s change, the MDS 3.0 data set will be undergoing the most significant change to the RAI since its implementation in 2010.
With this year’s change, the MDS 3.0 data set will be undergoing the most significant change to the RAI since its implementation in 2010.